Carbamazepine is a sodium channel blocker which reduces the permeability of nerve cell membranes to sodium and calcium ions. This decreases their inward flow. This prolongs the excitation phase of action potentials, reduces neuronal excitability, and inhibits neural transmission from the ventral anterior thalamic nucleus to the frontal lobe. Carbamazepine is used to treat epilepsy, peripheral neuropathic pain and psychiatric disorders. It is also used to prevent or treat depression, manic episodes, and insomnia. It also has antiarrhythmic properties. [2]As the expand of the clinical applications of carbamazepine, the case of misuse or its concurrent use with multiple medications have increased, leading to a gradual rise in adverse drug reactions (ADRs). In severe cases, these reactions may endanger patient safety.
Clinical Safety Application Cases of Carbamazepine
This article provides an in-depth analysis of a clinical case report published in Clinical Rational Drug Use. The report provides a detailed description of the diagnostic and therapeutic processes for an 87-year-old male patient who developed a drug reaction with eosinophilia and systemic symptoms (DRESS) after being administered carbamazepine. The case study emphasizes the crucial role of clinical pharmacy monitoring and pharmacogenomic testing in accurately identifying the cause of adverse reactions and making clinical decisions, providing important practical evidence for the clinical safe application of carbamazepine.
Core patient data and clinical progression
● Patient Basic Information: Male, 87 years old, with underlying conditions including post-cerebral infarction sequelae, cerebral atherosclerosis, hyperlipidemia, and Alzheimer's disease.
● Medication history: Carbamazepine tablets were added on 13 August 2022 to control epilepsy. There have been no further seizures since then.
● Timeline of Adverse Reactions:
〡Week 6 post-treatment (September 29th): Raised, wheal-like rashes developed on the upper limbs, protruding above the skin surface.
〡Week 7 post-treatment (October 5th): The rashes progressed and were accompanied by erythema and ulceration.
● Key laboratory indicator (eosinophil count):
〡Pre-treatment (August 16th): 0.08 × 10⁹/L (ratio 0.7%) — normal.
〡Following the onset of the rash on 20 October: The eosinophil count significantly increased to 7.05×10⁹/L (ratio 31.2%), far exceeding the normal range of 0.02–0.5×10⁹/L (0.5–5%).
〡After discontinuing medication (November 4th): the eosinophil count was 4.04×10⁹/L (ratio 35.3%).
〡Recovery phase (December 18th): Decreased to 1.29×10⁹/L (ratio 13.7%).
〡The dynamic changes in this indicator constitute key laboratory evidence for diagnosing DRESS.
The Core Role of Clinical Pharmacy Interventions and Genetic Testing
1.Precise identification and intervention:
During rounds on October 15th, the clinical pharmacist, exercising professional vigilance, linked the rash to carbamazepine and immediately recommended the following:
① Discontinuing carbamazepine;
②Conducting HLA gene testing. The physician adopted the recommendations and formally discontinued the medication on October 18th.
2.Genetic testing results provide molecular biological evidence:
Based on the warnings in the drug instruction and the PharmGKB database guidelines, the sample from patient was tested. The results indicate:
〡HLA-A*3101 allele: Heterozygous mutation positive.
〡This genotype shows moderate association with carbamazepine-induced hypersensitivity reactions (including SJS/TEN, maculopapular rash, and DRESS). This report genetically confirms the patient as a high-risk individual for severe adverse reactions to carbamazepine.
Discussion and In-Depth Academic Analysis
This case is academically valuable because it provides an excellent example of the modern precision medicine model, seamlessly transitioning from clinical phenomena to molecular mechanisms and ultimately guiding clinical practice.
1.Precise Diagnosis of Adverse Reactions:
This case meets the criteria for atypical drug hypersensitivity syndrome.
The diagnostic criteria for DIHS/DRESS are:
① Rash appearing >3 weeks after taking medicine;
② Markedly elevated eosinophils (>1.5 × 10⁹/L);
③ Accompanied by systemic symptoms (pruritus, fever). These criteria indicate a severe drug eruption, which can be distinguished from ordinary, mild eruptions.
2.Clinical Guidance Value of Pharmacogenomics:
This paper reiterates the recommendations of the U.S. FDA and Chinese guidelines: Prior to initiating carbamazepine therapy in Asian populations, screening for the HLA-B*1502 and HLA-A*3101 alleles is recommended. Patients testing positive for these alleles should be contraindicated for carbamazepine and advised to select alternative antiepileptic drugs, thereby preventing such severe, potentially fatal adverse reactions.
3.Expanded Role of Clinical Pharmacy: This case represents a prime example of "patient-centered" pharmaceutical care. Pharmacists transcended traditional functions by:
〡proactively monitoring and evaluating: identifying suspected adverse drug reactions (ADRs).
〡Providing evidence-based recommendations: Recommending genetic testing to provide objective diagnostic support.
〡Providing comprehensive pharmaceutical care: Participating in consultations and tracking treatment efficacy and laboratory indicators to ensure medication safety.
Conclusions and Clinical Implications
This case report clearly indicates:
●Severe cutaneous adverse reactions caused by carbamazepine, such as DRESS, SJS and TEN, have a long incubation period, rapid progression, and a high mortality rate. Therefore, they must be given high attention.
●For special populations, such as the elderly or those taking multiple medications, adhere to the principle of 'low initial dose with gradual titration' and enhance medication monitoring.
●Implementing 'pre-treatment genetic screening' is the most effective strategy for preventing such adverse events. This approach aligns with the principles of precision medicine, significantly enhancing medication safety and offering high clinical value and cost-effectiveness.
In summary, this case not only represents a successful treatment outcome, but also provides a valuable reference for clinical practitioners by demonstrating rational clinical medication and precision medicine practices.
References:
[1] 徐静,路瑶,郭丹丹,等.药师参与因卡马西平致皮疹不良反应1例的药学实践[J].临床合理用药,2025,18(18):163-166.DOI:10.15887/j.cnki.13-1389/r.2025.18.043.
[2] 夏益清.卡马西平不良反应[J].临床合理用药杂志,2011,4(17):80.DOI:10.15887/j.cnki.13-1389/r.2011.17.129.
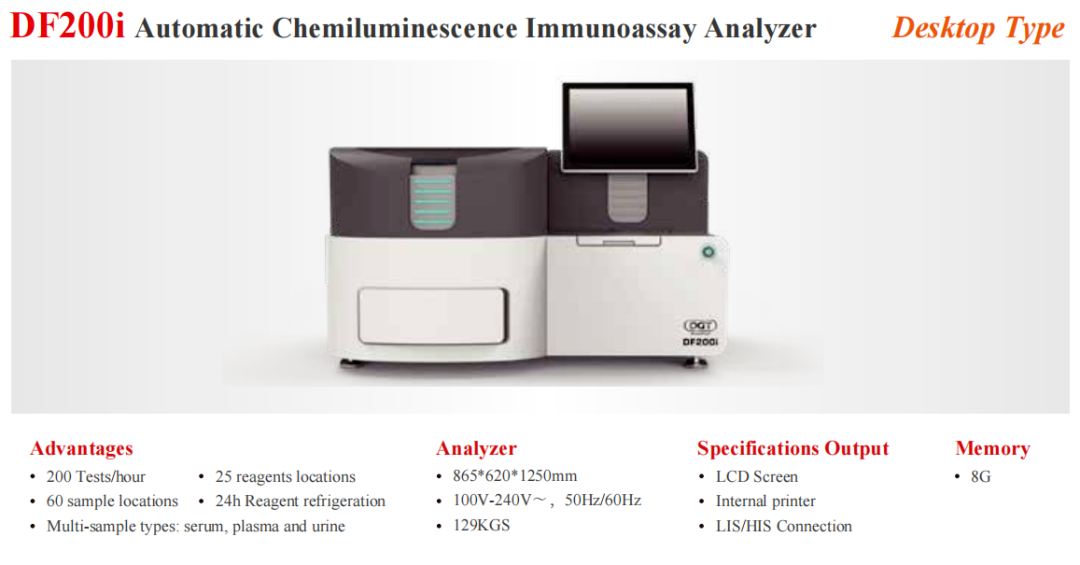
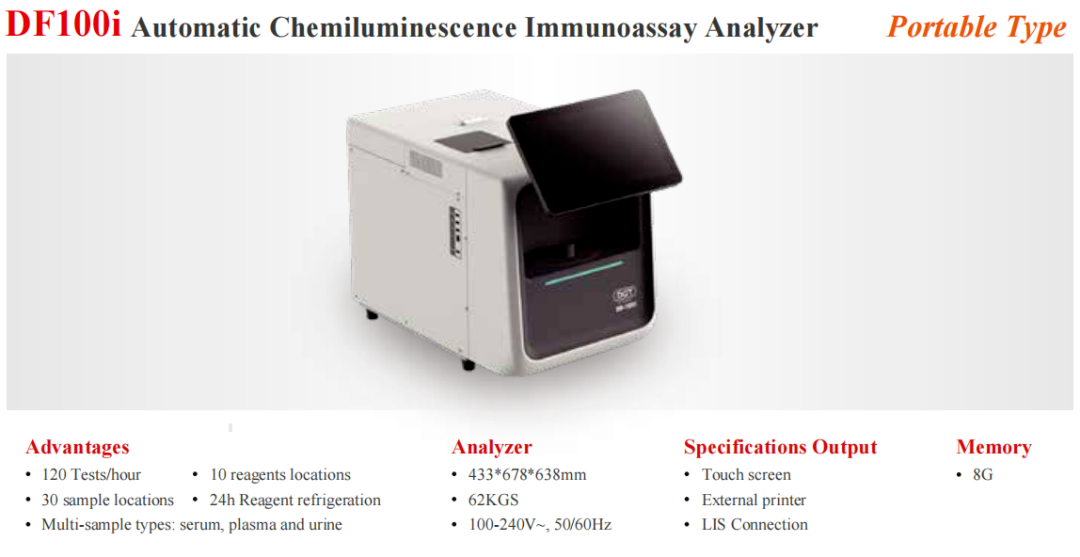
Automated Therapeutic Drug Monitoring Platformfor Chemicals and Biologics