Invasive fungal infections are becoming a deadly threat to high-risk populations, acting as the 'invisible killer' in critical care ICUs and the 'medication safety gatekeeper' after liver transplants. Voriconazole, the 'core mainstay' of clinical antifungal therapy, has frequently resulted in treatment complications due to soaring resistance rates and significant variations in blood concentrations[1]. The Voriconazole in vitro diagnostic reagent precisely addresses these clinical issues by using real-world data to circumvent resistance issues and control dosing, thus safeguarding the medication safety of critically ill ICU patients and transplant recipients. Its clinical necessity is undeniable!
I. Addressing critical pain points in high-risk scenarios: In Vitro Diagnostics Are Indispensable at These Moments
Invasive fungal infections are highly insidious and progress rapidly, particularly in settings like ICUs and transplant units. A single medication error can easily push mortality rates above 50%. The “uncertainty in voriconazole usage” further complicates clinical management. Real-world cases underscore the critical importance of diagnostic reagents.
◯ICU Critical Scenario: Misdiagnosis of Drug Resistance May Lead to Missed Lifesaving Window
ICU patients often have compromised immunity. The incidence of fungal infections exceeds 35%, compounded by ventilator use and the overuse of broad-spectrum antibiotics. These infections progress rapidly, and the mortality rate increases by 10% for every day that effective treatment is delayed.
A critically ill patient with sepsis complicated by an Aspergillus infection was admitted to a tertiary hospital ICU. Initial treatment with voriconazole for three days failed to improve the patient's condition; they remained febrile, with their respiratory failure worsening to the point of critical illness. Emergency in vitro diagnostic testing revealed complete resistance to voriconazole. The physicians immediately switched to a sensitive antifungal agent. Within three days, the patient's temperature had decreased, their symptoms had gradually resolved and their condition had stabilized.
Without precise testing, patients will only miss the golden window for effective intervention through ineffective care if they are subjected to blind reliance on empirical treatment, which could potentially endanger their lives.
◯Liver Transplant Scenario: Uncontrolled drug levels in the blood can easily trigger secondary liver damage.
Patients who have undergone a liver transplant exhibit incomplete restoration of liver function, resulting in significantly reduced voriconazole metabolism capacity. Their therapeutic window is 30% narrower than that of the general population — concentrations below 1.0 μg/mL may lead to treatment failure, while levels exceeding 4.4 μg/mL cause a sharp increase in hepatotoxicity. Given that the individual coefficient of variation in plasma drug concentration can be as high as 94%, relying solely on empirical dose adjustments carries a high degree of risk. Clinical data from a transplant centre indicates that, among liver transplant patients not undergoing therapeutic drug monitoring, the incidence of voriconazole-related hepatotoxicity was 28%. However, after implementing dynamic monitoring with in vitro diagnostic reagents and real-time dose adjustments, the hepatotoxicity rate fell to 8%[2].
One liver transplant recipient experienced a doubling of their transaminase levels three days after starting their initial medication. In vitro diagnostic testing revealed a blood drug concentration of 6.2 μg/ml, which far exceeded the safety threshold. After the physician promptly reduced the dose, the patient's blood drug concentration returned to a safe level, their transaminase levels gradually declined, and secondary liver damage was successfully prevented.
II. Popular Decoding of Core Advantages: Understand Its "Hardcore Strength" Without Professional Terminology
High-quality voriconazole IVD reagents can meet the needs of high-risk scenarios, with core advantages lying in "precision, speed, and full adaptability," which are easy to understand in plain language:
◯Ultra-high precision: Comparable to an "Antifungal Medication Navigator"
Relying on two core technologies, the matching degree between test results and clinical treatment effects exceeds 93%, almost avoiding misjudgment:
- Blood Concentration Detection:
Adopting ultra-high-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS, the clinical gold standard), it is like installing a "precision balance" for blood concentration, accurately measuring whether the concentration is within the safe range of 1.0~4.4 μg/ml, avoiding insufficient or excessive dosage;
- Fungal Drug Sensitivity Detection:
The consistency between the AST-YS08 susceptibility card and clinical reference methods is over 90%, which can clarify whether pathogenic bacteria are "sensitive" or "resistant" to voriconazole, directly helping doctors avoid drug resistance traps without blind trial medication[3]
◯Fast Speed: Seizing the "Golden Treatment Hour" for High-Risk Patients
Fully adapting to clinical emergency needs, the efficiency is doubled compared to traditional methods:
- Blood Concentration Detection:
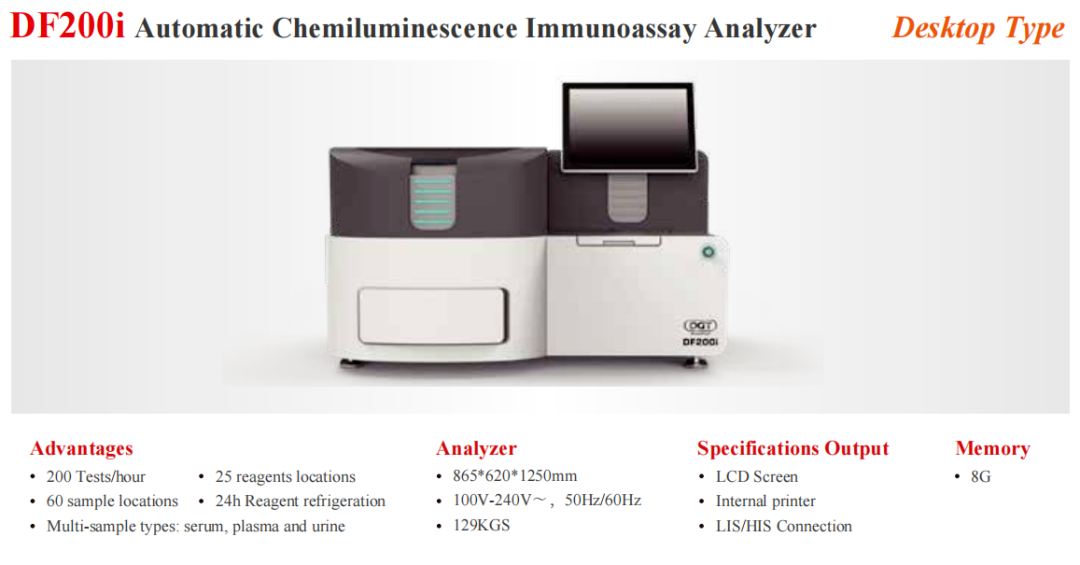
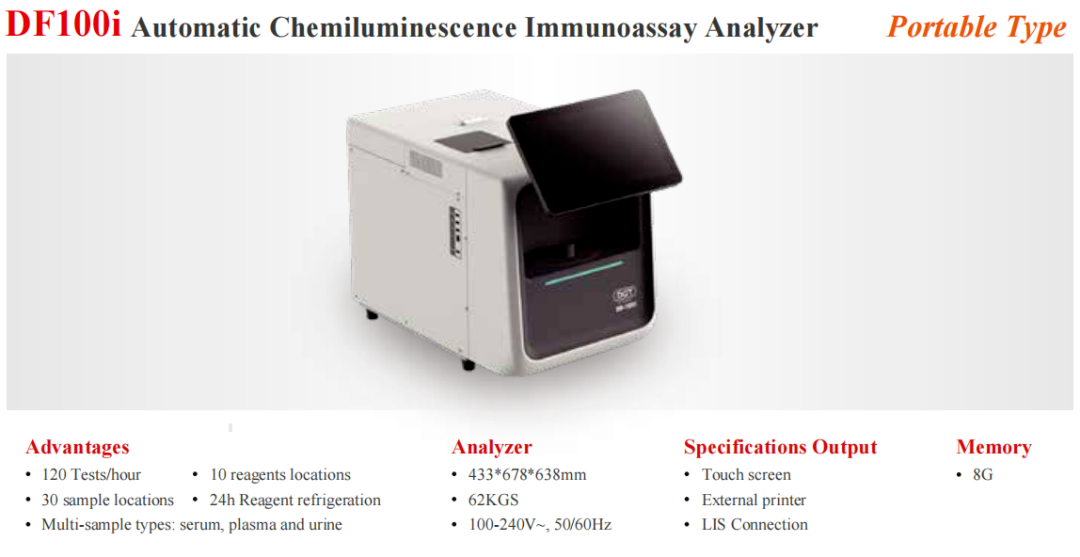
The chemiluminescent immunoassay (CLIA) can produce results within half an hour, eliminating the need for critically ill patients to wait for a long time;
- Fungal Drug Sensitivity Detection:
Drug resistance can be confirmed in around 13 hours, which is half the time taken by traditional testing methods. This enables doctors to develop treatment plans swiftly without delaying critical care.
◯Strong Adaptability: Covering All High-Risk Infection Scenarios
It is fully adaptable for emergency testing for critical infections in the ICU, long-term medication monitoring for liver and hematopoietic stem cell transplant patients, and routine fungal infection screening in respiratory and hematology departments. Primary care and tertiary hospitals alike can operate it — no complex equipment or specialized technical teams are required. Practicality at its best.
III. Elevation of Clinical Value: The Leap from "Empirical Trial Medication" to "Precision Treatment"
From improving the outcomes for critically ill ICU patients to ensuring the safe use of medication after liver transplants, voriconazole in vitro diagnostic reagents are transforming traditional antifungal treatment models. By replacing subjective experience with objective data, they enable clinicians to avoid the pitfalls of drug resistance and control blood drug concentrations precisely. This approach significantly increases treatment success rates and minimizes the risk of adverse reactions such as hepatic toxicity.
For high-risk patients, this test is not optional, but essential. For clinicians, it is a precision tool that assists in antifungal therapy, ensuring that every medication decision is evidence-based and effective. This fortifies the lifeline of protection for vulnerable populations.
References:
[1] 王辰, 李建国. 伏立康唑在ICU重症真菌感染患者中的精准用药研究[J]. 中国危重病急救医学, 2024, 36(5):489-493.
[2]刘俊兰,宋燕,张洁,等.伏立康唑在肝移植术后感染患者中的治疗药物监测[J].中华检验医学杂志, 2025, 48(03): 346-351.
[3] 朱永泽,吕火祥,胡庆丰,等.伏立康唑体外真菌药敏试验两种方法对比研究[J].中国卫生检验杂志, 2009(4):2.
Automated Therapeutic Drug Monitoring Platformfor Chemicals and Biologics