Ovarian cancer (OC) is the eighth leading cause of cancer death among women worldwide. Over two-thirds of patients are diagnosed at an advanced stage, which carries a high risk of recurrence and low five-year survival rates [1–3]. Angiogenesis is a critical pathway for tumour growth and metastasis. Bevacizumab, the first monoclonal antibody to target vascular endothelial growth factor (VEGF), is a core targeted therapy in the treatment of advanced ovarian cancer (AOC) [4]. This study conducted a systematic review of the efficacy and safety data of bevacizumab in first-line, maintenance and recurrence treatments, with the aim of clarifying its clinical value in different risk groups and treatment lines. This provides evidence for precision medicine [5].
Findings and Data Support
Efficacy performance across different treatment scenarios
● First-line treatment setting:
Based on the results of the GOG-0218 and ICON-7 phase III trials, the standard regimen for newly diagnosed advanced ovarian cancer is maintenance bevacizumab therapy following platinum-based chemotherapy [6-9]. The real-world RESPONSE study further confirmed that maintenance therapy significantly improves overall patient survival (HR=0.62, 95% CI=0.42–0.91, p=0.01) [10]. However, the BOOST trial indicated that extending the duration of treatment beyond 30 months did not provide any additional benefit, and that 15 months was the optimal duration [11].
● Recurrent treatment setting:
Bevacizumab has been shown to be effective in treating both platinum-sensitive and platinum-resistant recurrent cases. In the AURELIA Phase III trial, median progression-free survival (PFS) for platinum-resistant patients receiving combination chemotherapy increased from 3.4 months to 6.7 months (hazard ratio (HR)=0.48, 95% confidence interval (CI)=0.38-0.60, p<0.001), and crossover use after disease progression reduced the risk of death further [12,13]. In platinum-sensitive patients, the GOG-0213 trial demonstrated median PFS of 13.8 months with combination chemotherapy plus maintenance therapy (HR=0.63, p<0.0001) [20], and the OCEANS trial confirmed that maintenance therapy significantly prolonged PFS (12.4 months vs. 8.4 months, HR=0.48, p<0.0001) [14,15].
● Re-challenge setting:
Bevacizumab remains effective when re-administered after disease progression. In the JGOG3023 Phase II trial, the median PFS for recurrent platinum-resistant patients receiving re-challenge therapy increased from 3.1 months to 4.0 months (HR = 0.54, 95% CI = 0.32–0.90, p = 0.0082). The MITO16b/MANGO-OV2/ENGOT-ov17 phase III trial demonstrated a median progression-free survival (PFS) of 11.8 months in patients with platinum-sensitive recurrent disease who received rechallenge therapy (hazard ratio [HR] = 0.51, p < 0.0001) [16]. Combination with PARP inhibitors: The PAOLA-1 Phase III trial confirmed the significant efficacy of bevacizumab plus olaparib in patients with homologous recombination deficiency (HRD), with a median PFS of 46.8 months (HR = 0.41, 95% CI = 0.32–0.54), including a median PFS of 60.7 months in patients with a BRCA mutation [5, 17]. This combination has been approved as a first-line maintenance therapy for HRD-positive advanced ovarian cancer [18,19]. The OVARIO Phase II trial demonstrated a median PFS of 28.3 months for bevacizumab plus niraparib in HRD-positive patients [20].
Risk stratification and biomarkers for target populations
● Risk Stratification Breakthrough:
While it was previously thought that bevacizumab only benefited high-risk patients, a post-hoc analysis of the PAOLA-1 trial revealed that low-risk patients (stage III with complete resection) who received olaparib maintenance therapy achieved a five-year progression-free survival rate of 72%. This was significantly higher than the 28% achieved by the bevacizumab monotherapy group [21]. Furthermore, the ICON-7 trial's imaging analysis demonstrated that the efficacy of bevacizumab is unaffected by risk stratification [22].
● Biomarker guidance:
HRD status is a core prognostic indicator. Patients with HRD demonstrate a significant benefit, whereas those without HRD show no clear advantage (HR = 1.01, 95% CI = 0.77–1.33) [17]. The KELIM score (based on CA-125 clearance rate) is used to assess chemotherapy sensitivity. Patients at high risk with a score of less than 1.0 (chemotherapy-insensitive) demonstrate greater overall survival (OS) benefit with bevacizumab [23, 24].
The safety profile of bevacizumab is based on data from over 5,700 patients with malignant tumours, which demonstrates generally good tolerability [25]. Common adverse reactions include hypertension, fatigue, diarrhoea and abdominal pain, predominantly grades 1–2 [6,12,26]. The incidence of hypertension and proteinuria is lower when bevacizumab is combined with olaparib than with bevacizumab monotherapy [5, 27]. Serious adverse reactions are uncommon, with gastrointestinal perforation occurring in 3% of patients during first-line treatment and less than 2% during recurrent treatment [6,26]. Risk factors include a history of diverticulitis and abdominal abscesses [28]. Elderly patients (aged ≥70 years) exhibit a slightly higher incidence of hypertension, but their overall toxicity profiles show no significant difference compared to those of younger patients [29,30]. (For a summary of the experiments, see the table below)


Research Findings and Clinical Implications
Bevacizumab has been shown to provide significant benefits throughout the entire treatment cycle of advanced ovarian cancer, including first-line maintenance therapy, treatment for recurrence, and re-challenge therapy. It is particularly valuable for HRD-positive patients. Contrary to the previous limitation that it only benefits high-risk patients, HRD-positive low-risk patients can also achieve long-term survival benefits from bevacizumab combined with PARP inhibitors, with a remarkable 5-year progression-free survival rate [21]. Bevacizumab has a favourable safety profile, with preventable and manageable adverse reactions. Its safety profile is further enhanced when combined with PARP inhibitors, making it suitable for long-term maintenance therapy.
● Treatment Decision Optimisation:
For HRD-positive patients, the preferred recommendation is bevacizumab combined with olaparib maintenance therapy. In the absence of clear biomarkers, both low- and high-risk patients may be considered for treatment. High-risk patients scoring <1.0 on the KELIM score demonstrate greater benefit [23,24]. Timing of therapy: Prioritise bevacizumab in first-line treatment to maximise survival benefit; re-challenge therapy may be considered after disease progression [31,32]. Safety Management: Assess risk factors such as gastrointestinal perforation and cardiovascular disease prior to administration. Blood pressure and urine protein should be regularly monitored during treatment; patients with hypertension must achieve blood pressure control before therapy is initiated [25,33].
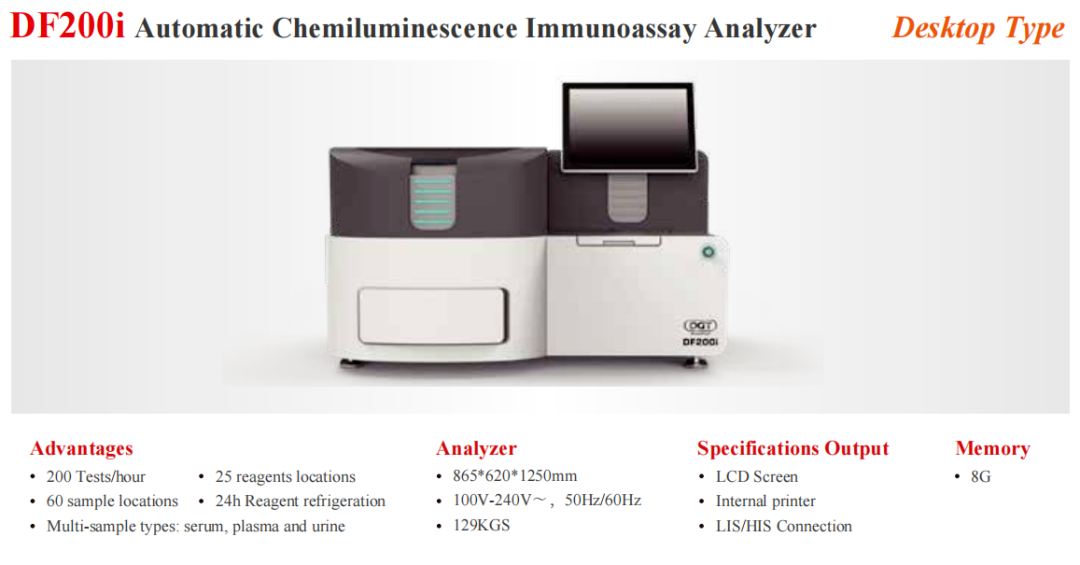
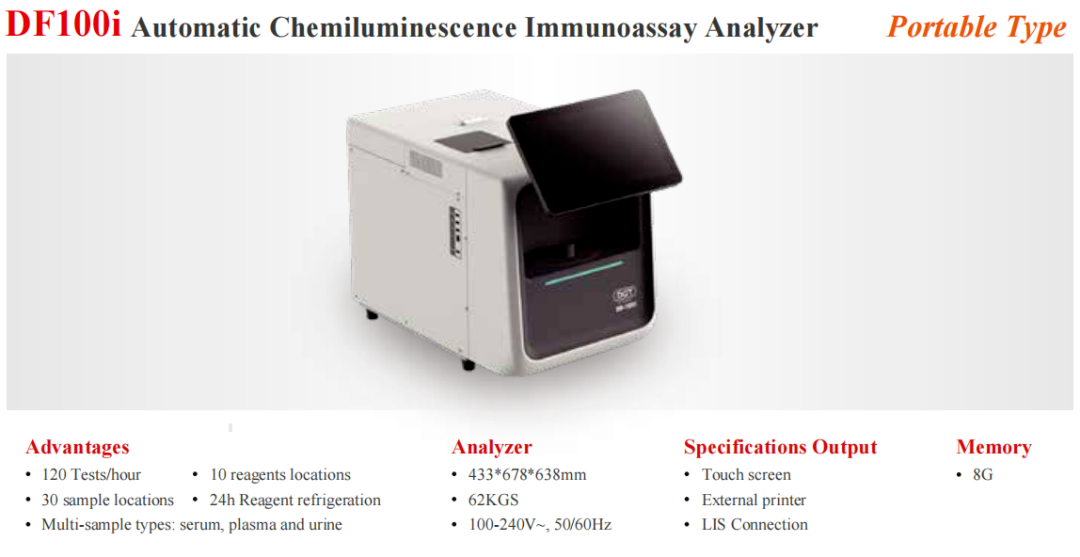
Automated Therapeutic Drug Monitoring Platformfor Chemicals and Biologics