Children are susceptible to lead pollution. Lead poisoning can cause irreversible damage to multiple organs and systems in children. Lead will affect children's brain development, causing a decrease in intelligence quotient (IQ). For every 12 μg/L increase in blood lead in children, cognitive ability will decrease by 1 point [1]. Children's behavior of chewing toys or fingers results in their lead intake far exceeding that of adults, which is about 4 to 5 times that of adults.
Compared with adults, infants and young children have a higher absorption rate of the ingested lead, with the absorption rate being approximately 50% of the ingested amount. At the same time, children's ability to excrete lead is much lower than that of adults [2].
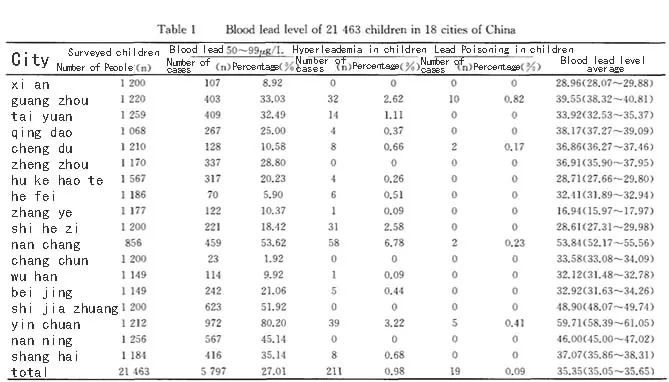
According to research [3], the overall average blood lead value of urban children in China is 35.35±1.87 μg/L, and 1.07% of children have blood lead levels greater than 100 μg/L. The overall situation is not optimistic and still needs the attention of the whole society.
Even if children are lead poisoned, the clinical symptoms are relatively unclear,
and blood lead concentration detection is a reliable method of diagnosing lead-exposed individuals.
In order to ensure that children grow up safely in a lead-free environment,
children’s blood lead levels need to be tested regularly.
Find and stay away from sources of lead exposure promptly.
It is estimated [4] that of the 2 million people who died from exposure to known chemicals in 2019,
nearly half were caused by lead exposure. Because lead exposure has long-term health effects, including
30% of the global burden of idiopathic intellectual disability,
4.6% of the global cardiovascular disease burden,
and 3% of the global chronic kidney disease burden.
High levels of lead exposure in pregnant women can lead to miscarriage, stillbirth, premature birth and low birth weight. Therefore, adults, especially pregnant women, should also undergo regular blood lead testing to rule out potential disease risks.
Blood lead concentration testing and management indicators
2006 Ministry of Health "Principles for Classification and Treatment of Hyperleademia and Lead Poisoning in Children"When children's blood lead levels are above 100 μg/L, it’s necessary to carefully inquire about the pollution status of the living environment and whether family members and companions have a history of long-term lead exposure and lead poisoning.
2022 Ministry of Health "Blood Lead Reference Limit Standards for Children Aged 0-6" (Draft for Comments)
50 μg /L is used as the reference limit for high blood lead levels caused by lead exposure in children. When two consecutive blood lead (at least one venous blood lead) test values are ≥50 μg/L, and the time interval between the two consecutive tests does not exceed 1 month, it should be considered that the child's blood lead level is high.
2022 WHO “Guidelines for the Clinical Management of Lead Exposure”
For individuals with blood lead concentrations ≥ 50 µg/L, the source of lead exposure should be identified and appropriate actions taken to reduce and terminate exposure.
2021 U.S. Centers for Disease Control and Prevention "CDC updates blood lead reference value to 3.5 µg/dL"
After the blood lead reference value is updated to 35 μg /L, children with blood lead levels in the range of 35-50 μg/L can now take timely measures to reduce the impact on health and eliminate or control sources of exposure.
There is no known safe blood lead level. Therefore, the prevention of lead exposure is particularly important.
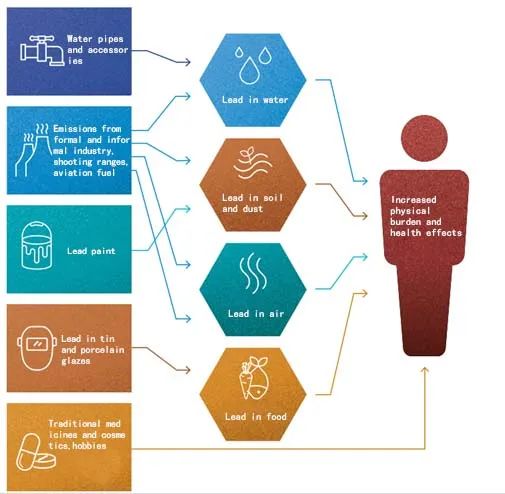
Major sources and routes of lead exposure
There are many sources and routes of lead exposure. The most important routes of exposure to lead and its compounds are ingestion and inhalation. Most cases of oral lead poisoning result from the regular ingestion of small amounts of lead-containing materials (such as contaminated dust or soil, lead-based paint flakes, contaminated food and spices, lead-containing traditional medicines) or cause by the ingestion of lead-containing foreign bodies [5].
As of July 2021, leaded fuel for cars and trucks is no longer sold around the world [6], which has proven to have significant public health benefits.
Prevention of lead poisoning in children
Strengthen health education measures,
promptly correct children’s bad habits in daily life,
pay special attention to children's hand hygiene, pay attention to lead contamination in daily necessities, and avoid staying in areas with a lot of lead dust.
It can avoid the possible damage caused by lead to children to the greatest extent [7].
Diagreat Biotech’s blood lead concentration rapid detection solution
The blood lead concentration detection item, a key project of Diagreat Biotech's POCT platform, can quickly detect human blood lead levels, indicate the human body's lead exposure level, facilitate early intervention by doctors, and help protect children's healthy growth in a lead-free environment. This method has obtained Chinese patent (Patent No.: 201910916128.5) and US patent (Patent No.: GWP201907402). Compared with the traditional graphite furnace atomic absorption spectrometry or flame atomic absorption spectrometry, Diagreat uses POCT fluorescence immunochromatography for rapid detection of heavy metal lead with obvious advantages: the instrument is portable, safe (no flammable gas required), simple (no sample pretreatment), low running costs and small sample volume required (20 μL).
In addition to lead, the heavy metal cadmium is also included in our testing items.
Safe, convenient and fast
【References】
[1] Lanphear BP, Hornung R, Khoury J, et al. Low-level environmental lead exposure and children's intellectual function: an international pooled analysis [J]. Environ Health Perspect, 2005, 113(7): 894-899.
[2] World Health Organization. Brief guide to analyticalmethods for measuring lead in blood, second edition. Geneva: World Health Organization, 2020.
[3] Liu Aihua,
Li Tao,
Zhang Shuaiming,
et al.
Current status of blood lead levels and influencing factors among children in 18 cities in China [J]. Chinese Maternal and Child Health Research, 2018, 29(5): 539-542.
[4] World Health Organization. The public health impact of chemicals: knowns and unknowns. Geneva: World Health Organization, 2021.
[5] World Health Organization. WHO guideline for the clinical management of exposure to lead. Geneva: World Health Organization, 2022.
[6] Angrand RC, Collins G, Landrigan PJ, et al. Relation of blood lead levels and lead in gasoline: an updated systematic review [J]. Environ Health, 2022, 21(1): 138.
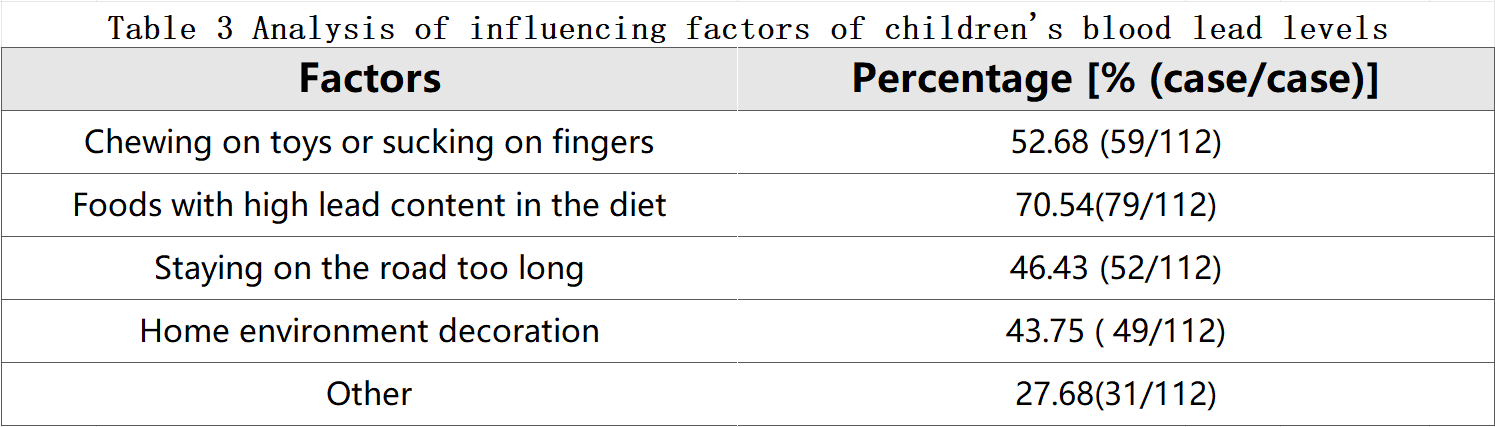
[7] Deng Mei.
Determination of blood lead levels in children and analysis of influencing factors [J]. Journal of Practical Laboratory Physicians, 2018, 10(2): 85-87.