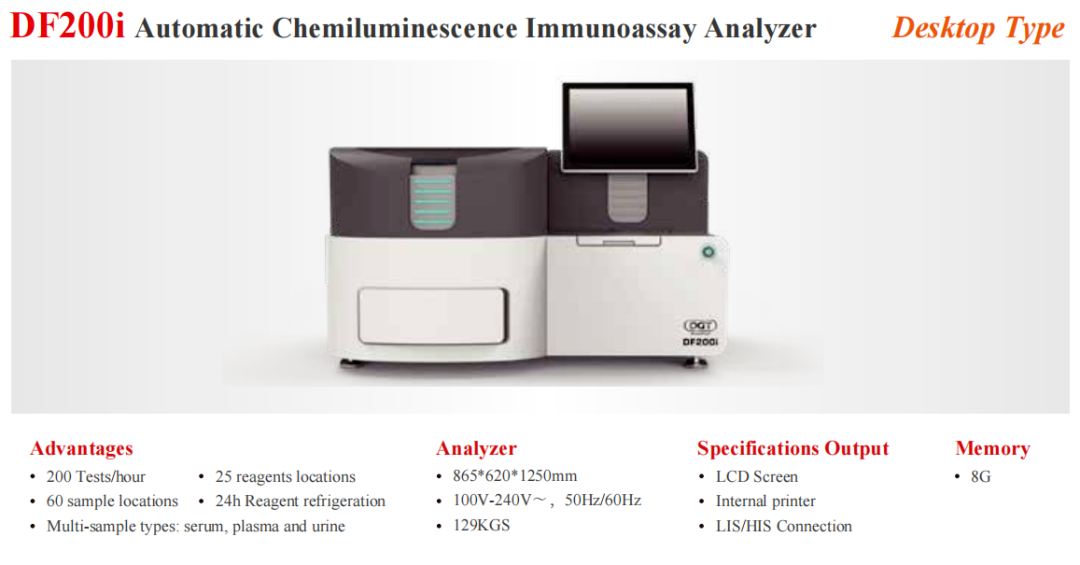
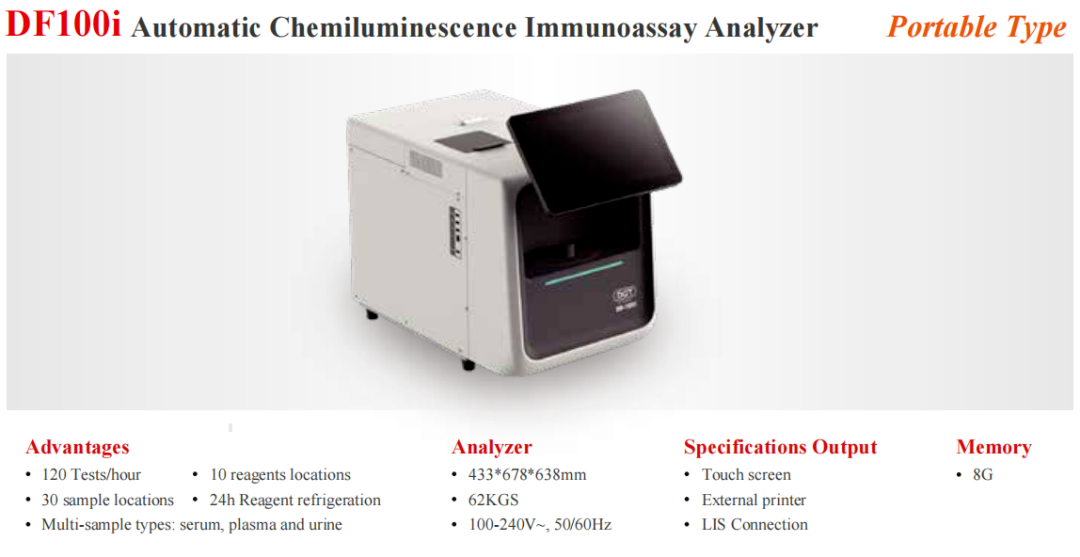
Diagreat has innovatively developed the Paclitaxel Detection Kit (Chemiluminescence Immunoassay), which can simultaneously detect Paclitaxel Injection, Paclitaxel Liposome, and Paclitaxel Albumin Bound, three different preparation types of Paclitaxel, to meet the testing needs of clinical patients. At the same time, by carrying a fully automated chemiluminescence immunoassay analyzer, it is convenient and fast to realize TDM detection, providing TDM solutions for the precise treatment of patients, and scientifically realizing individualized medication[11].
参考文献
[ 1 ] Wang J,Lou P,Lesniewski R,et al. Paclitaxel at ultra low concentrations inhibits angiogenesis without affecting cellular microtubule assembly[J]. Anticancer Drugs,2003, 14(1):13.
[ 2 ] Chen Y,Pandya KJ,Feins R,et al. Toxicity profile and pharmacokinetic study of a phase I low-dose schedule-dependent radiosensitizing paclitaxel chemoradiation regimen for inoperable non-small cell lung cancer(NSCLC) [J]. Int J Radiat Oncol Biol Phys,2008,71(2):407.
[ 3 ] Campone M,Levy V,Bourbouloux E,et al. Safety and pharmacokinetics of paclitaxel and the oral mTOR inhibitor everolimus in advanced solid tumours[J]. British Journal of Cancer,2009,100(2):315.
[ 4 ] van de Steeg E,van Esch A,Wagenaar E,et al. High impact of Oatp1a/1b transporters on in vivo disposition of the hydrophobic anticancer drug paclitaxel[J]. Clin Cancer Res,2011,17(2):294.
[ 5 ] Steed H,Sawyer MB. Pharmacology,pharmacokinetics and pharmacogenomics of paclitaxel[J]. Pharmacogenomics. 2007,8(7):803.
[ 6 ] 李苏,廖海,詹靖,等.比较白蛋白纳米紫杉醇与含聚氧乙烯蓖麻油紫杉醇在乳腺癌患者的药代动力学[J].中国临床药理学杂志,2010,26(8):606.
[ 7 ] 杨莹,曹丰.国产紫杉醇在患者血浆中的药代动力学及临床观察[J].中国肿瘤临床与康复,2008(3):70.
[ 8 ] Joerger M,Huitema AD,Huizing MT,et al. Safety and pharmacology of paclitaxel in patients with impaired liver function:a population pharmacokinetic-pharmacodynamic study[J]. British Journal of Clinical Pharmacology, 2007,64(5):622.
[ 9 ] Joerger M,Huitema AD,van den Bongard DH,et al. Quantitative effect of gender,age,liver function,and body size on the population pharmacokinetics of Paclitaxel inpatients with solid tumors[J]. Clin Cancer Res,2006,12(7):2150.
[ 10 ] 滕雪,吴东媛,刘爽,董梅.紫杉醇的治疗药物监测研究进展[J].中国药房,2014,25(48):4598-4601.
[ 11 ] 武渊,张琰,彭伟等.紫杉醇血药浓度监测在乳腺癌新辅助治疗中的临床应用[J].南京医科大学学报(自然科学版),2018,38(05):681-683.